In the past few years, state and local governments across the U.S. have begun spending billions in opioid settlements paid by companies accused of fueling the overdose crisis. But where is that money going, who is getting it, and is it doing any good?
KFF Health News, partnering with the Johns Hopkins Bloomberg School of Public Health and Shatterproof, a national nonprofit focused on addiction, undertook a yearlong investigation to find out.
Dozens of interviews, thousands of pages of documents, an array of public records requests, and outreach to all 50 states resulted in a first-of-its kind database that catalogs more than 7,000 ways opioid settlement cash was used in 2022 and 2023. It’s the most comprehensive resource to date tracking some of the largest public health settlements in American history.
Among the findings:
- States and localities received more than $6 billion in opioid settlement funds in 2022 and 2023. According to public records, they spent or committed about a third of that amount and set aside about another third for future use. The final third was untrackable, as many jurisdictions did not produce public reports on the funds.
- Reports of spending tracked the minuscule to the monumental, from $11.74 to buy postage in Yavapai County, Arizona, to more than $51 million to increase the addiction treatment workforce in California.
- States allotted, on average, about 18% of their funds for addiction and mental health treatment; 14% for recovery services such as housing, transportation, and legal aid; 11% for harm reduction efforts such as overdose reversal medications; and 9% for prevention programs that aim to stop people from developing substance use disorders. States committed, on average, about 2% for syringe service programs, through which people can get sterile needles. (A variety of entities received this money, from law enforcement to nonprofit organizations to government agencies.)
- Governments reported spending more than $240 million on purposes that did not qualify as opioid remediation. (Most settlements allow states to spend up to 15% of their funds this way.) Most of this tranche went to legal fees, but several jurisdictions funneled money to their general fund. One county even sent funds to its road and bridge department.
- Several cities and counties reported expenditures they said addressed the overdose crisis but that would leave an average person scratching their head — such as $33.07 to an anti-abortion pregnancy center in Sandborn, Indiana, and $30,362 to screen first responders for heart disease in Oregon City, Oregon.
“When people know that people aren’t watching and there’s no accountability, then they can kind of do what they want,” said Tonja Myles, a community activist in Baton Rouge, Louisiana, who is in recovery. “That’s why we have to have some kind of database and accountability.”
Despite the recent decline in overall overdose deaths in the U.S., more than 90,000 people still died in the 12 months ending July 2024 and rates are rising in many Black and Native American communities.
“We can’t mess up or miss this moment,” Myles said.
Opioid settlement payouts are expected to total about $50 billion over nearly two decades, paid by more than a dozen companies that made or distributed prescription painkillers, including Johnson & Johnson, Walgreens, and Walmart. Although it’s a large sum, it’s dwarfed by the size of the crisis, making each dollar that’s spent critical.
KFF Health News and its partners reviewed hundreds of settlement spending reports, extracting expenditures line by line, and developed a methodology to sort the expenditures into categories like treatment or prevention. States were given an opportunity to review the data and comment on their spending.
To be sure, the database does not capture the full picture of opioid settlement spending nationwide. Some places do not publish spending reports, while others declined to engage with this project. The data presented here is a snapshot as of the end of 2023 and does not account for further spending in 2024. The differences in how states control, process, and report on the money make apples-to-apples comparisons nearly impossible. Still, the database helps fill a gap left by a lack of national reporting requirements and federal government inaction.
It is “a tool for those who want to objectively measure whether everything that can be done is being done,” said Matthew Myers, a former president of the Campaign for Tobacco-Free Kids, which compiles similar annual reports on tobacco settlement money.
Treatment a Clear Winner
The top priority to emerge from early opioid settlement spending was treatment, with more than $416 million spent or committed to residential rehabs, outpatient counseling, medications for opioid use disorder, and more.
The state of New York — which spent the most on treatment — allocated about $22 million of that for programs that make the gold standard for care as easy as possible for patients: providing same-day prescriptions for buprenorphine, a medication that decreases cravings for opioids.
The result was a program that John Greene said changed his life.
Greene, 57, used to live in the woods down the street from Family & Children’s Counseling Services in Cortland, New York. He cycled through jails and hospitals, overdosing half a dozen times and trying rehab just as many.
But now he has four months of recovery under his belt — the longest stint since he started regularly using drugs at 14.
He said it’s because the counseling center’s new program — funded by a mix of state and local opioid settlement dollars — has a different approach. Counselors aren’t didactic and judgmental. They don’t force him to stop smoking marijuana. Several staff members have experienced addiction themselves. They drive Greene, who doesn’t have a car, to doctor appointments and the pharmacy for his buprenorphine prescription.
Now Greene lives and works with his brother, looks forward to weekly counseling sessions, and is notching small victories — such as buying his nephew toy cars as a stocking stuffer.
“It made me feel good to do something for somebody and not expect nothing back,” Greene said.
Emily Georgia, one of Greene’s counselors, said the center has worked with nearly 200 people like him in the past year. Without the settlements, “the program probably wouldn’t exist,” she said.

Across the country, the money supports other innovative treatment approaches:
- $21 million for a new program in Kentucky that diverts people with mental illness or addiction who face low-level charges away from incarceration and into treatment, education, and workforce training
- More than $3 million for, in part, three new mobile methadone programs in Massachusetts, to bring the medication to rural and underserved areas
- Tens of thousands of dollars each in Iowa and Pennsylvania to cover out-of-pocket treatment costs for people without insurance or those with high deductibles
Philip Rutherford, an expert on substance use disorder at the National Council for Mental Wellbeing, said these efforts “are really positive” and many have been “historically difficult or impossible to achieve with federal or state funding.”
But some funds are also flowing to treatment approaches that defy best practices, such as denying people medications for opioid use disorder.
Some in the recovery community consider methadone and buprenorphine a crutch. But study after study show that the medications help people stay in treatment and reduce the risk of overdose and death. Research even suggests that treatment without these medications can be more harmful than no treatment at all.
Although not everyone will want medication, settlement funds shouldn’t “prop up a system that doesn’t allow people to have that choice,” said Regina LaBelle, a professor of addiction policy at Georgetown University.
Babies, Forgotten Victims of the Epidemic
While treatment received a windfall in early opioid settlement spending, another aspect of the crisis was neglected: neonatal abstinence syndrome, a condition in which babies exposed to drugs in the womb experience withdrawal.
Nationwide, more than 59 newborns a day are diagnosed with it. Yet only about $8.4 million in settlement money was committed to the issue — less than 0.5% of all funds publicly reported as spent or committed in 2022 and 2023.
Experts in public health and addiction, as well as affected families, say it’s due to stigma.
“A mom using drugs and being a parent is a very uncomfortable reality to face,” said Ashley Grant, a 38-year-old mother of three in Mesa, Arizona. “It’s easier to just push it under the rug or let them fall through the cracks, as sad as that is.”
It almost happened to her.
Grant learned she was pregnant with her third child last year. At the time, her partner was in jail and she was using drugs after an eight-year period of recovery, was estranged from her family, and didn’t know how she’d survive the next nine months.
During a visit to a methadone clinic, she saw a booth about Jacob’s Hope, a specialty nursery that cares for substance-exposed newborns and their moms. Nursery staff connected her with a therapist, helped her enroll in parenting classes, and dropped off diapers and a playpen at her home.

After delivering at the hospital, Grant and her baby boy stayed at Jacob’s Hope for about a week. Nurses showed her how skin-to-skin contact calmed his withdrawal symptoms and more frequent feedings and burpings decreased gastrointestinal discomfort, which is common among substance-exposed newborns.
Today, Grant has roughly five months of recovery. She got certified as a peer recovery specialist and hopes to join Jacob’s Hope one day to help moms like her.
But the nursery’s future is uncertain.
After opening in 2019, Jacob’s Hope nearly shut down this summer due to low reimbursements and delayed payments from insurers, said Lyndsey Steele, its associate director. Community donations kept the nursery afloat, but “it’s still hanging on by a thread,” she said.
She’s hoping opioid settlement money can help.

In 2022, Jacob’s Hope received about $250,000 from Arizona’s opioid settlements. But this year, the legislature captured the state’s share of remaining funds and, in a controversial move, gave it to the Department of Corrections.
Jacob’s Hope has now turned to local governments, which control their own settlement dollars. Its home city of Mesa said a first round of grant applications should open in the spring.
Steele prays it won’t be too late for babies in need — the epidemic’s “forgotten victims,” she called them.

Heart Disease Screening, Robot Ambulances, and More
Some opioid settlement expenditures have sparked fierce disagreement. They generally fall into three buckets: money for law enforcement, funding for youth prevention programs, and purchases unrelated to the opioid crisis.
Settlement dollars nationwide have bought body scanners, K-9 units, bulletproof vests, patrol trucks, and laptops and printers for police and sheriffs.
Some spending strayed even further from the spirit of the settlement. In Oregon City, Oregon, more than $30,000 was spent on screening first responders for heart disease. Police Chief Shaun Davis said his staff respond to opioid-related emergencies and experience trauma that increases their risk of heart attack.
But some people question if settlement funds should be footing the bill.
“This looks to me like you’re trying to defray other costs” from the police budget, said Stephen Loyd, chair of Tennessee’s Opioid Abatement Council. “I don’t think that there’s any way that this opioid money was earmarked for stuff like that.”
A second area of contention is youth prevention.
Although most people agree that stopping children from developing addictions is important, the execution is tricky.
Nearly half a million settlement dollars have gone to the Drug Abuse Resistance Education program, commonly known as D.A.R.E. Decades of research suggest its original curriculum is ineffective.
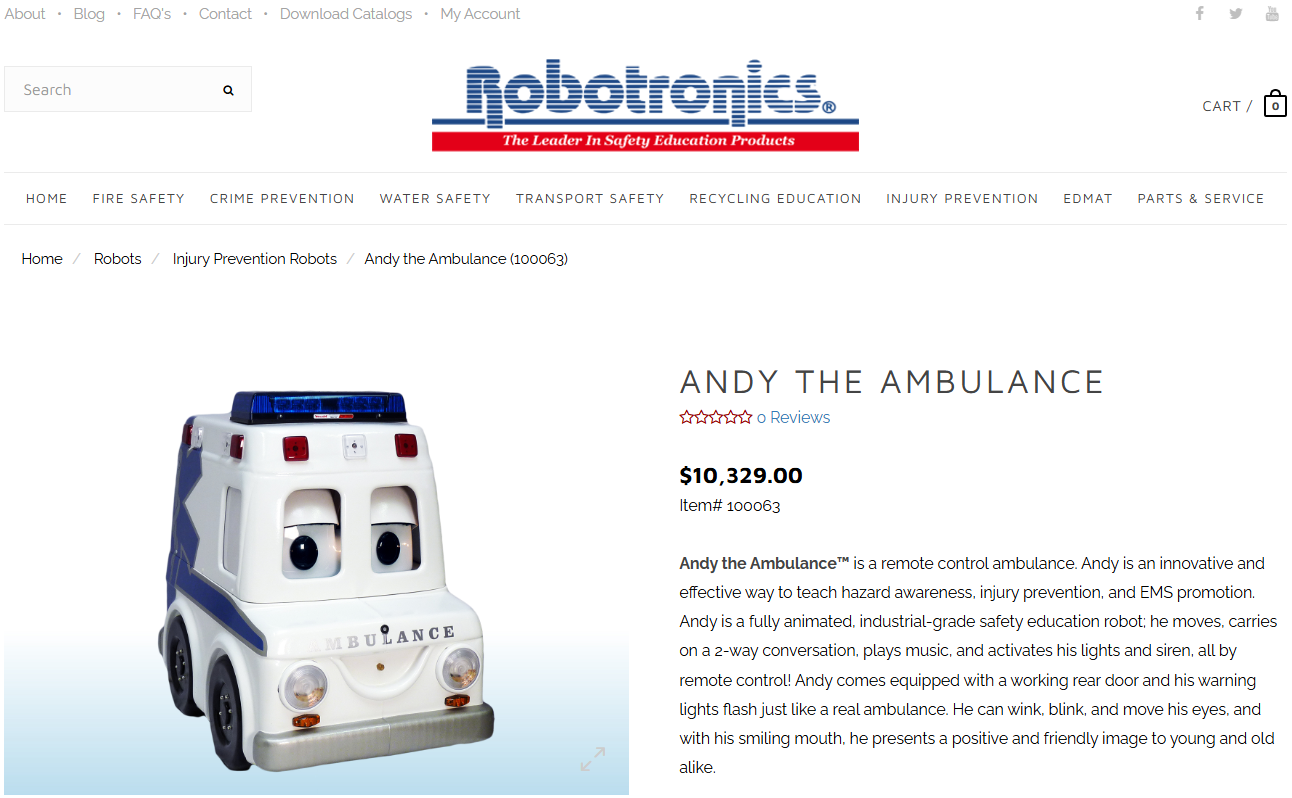
Robeson County, North Carolina, spent about $10,000 in settlement money to buy “Andy the Ambulance,” a robot ambulance with big eyes and an audio system through which a human operator can discuss the dangers of drugs. EMS Director Patrick Cummings said his team has taken the robot to churches and elementary schools.
We “don’t have any studies that show it’s working,” he said, but educating kids seems like a good investment because “if they never try it, they don’t get addicted.”
Then there’s the chunk of money — up to 15% of each state’s funds — that’s a free-for-all.
Flint, Michigan, spent nearly $10,000 on a sign for a community service center. The city reported that the expense did not qualify as “opioid remediation.” In other words, it’s unrelated to addressing the crisis.
But Caitie O’Neill, a city spokesperson, said that “the building sign makes it possible for residents to find” the center, which houses city services, “including Narcan kits, fentanyl testing strips, and substance abuse referrals.”

Jurisdictions across 29 states reported non-remediation spending in 2022 and 2023. Most opioid settlements require such reports but operate on an honor system. No one is checking if the other 21 states and Washington, D.C., were truthful.
Jackie Lewis, an Ohio mother whose 34-year-old son, Shaun, died of an overdose in October 2022, finds that hard to stomach.
“This is blood money,” she said. Some people have “lost sight of that.”
Lewis is raising Shaun’s daughter, ensuring the 9-year-old receives counseling at school and can attend the hip-hop music classes she enjoys — all on Lewis’ Social Security payments. This year they moved to a smaller town with lower costs.
As settlement funds continue flowing, she wants officials in charge of the money to help families like hers.
“We still exist and we’re still struggling,” she said.

KFF Health News’ Henry Larweh and Megan Kalata, Johns Hopkins Bloomberg School of Public Health’s Sara Whaley and Vivian Flanagan, and Shatterproof’s Kristen Pendergrass and Sahvanah Prescott contributed to this article.
The Johns Hopkins Bloomberg School of Public Health has taken a leading role in providing guidance to state and local governments on the use of opioid settlement funds. Faculty from the school collaborated with other experts in the field to create principles for using the money, which have been endorsed by over 60 organizations.
Shatterproof is a national nonprofit that addresses substance use disorder through distinct initiatives, including advocating for state and federal policies, ending addiction stigma, and educating communities about the treatment system.
Shatterproof is partnering with some states on projects funded by opioid settlements. KFF Health News, the Johns Hopkins Bloomberg School of Public Health, and the Shatterproof team who worked on this report are not involved in those efforts.

