[ad_1]
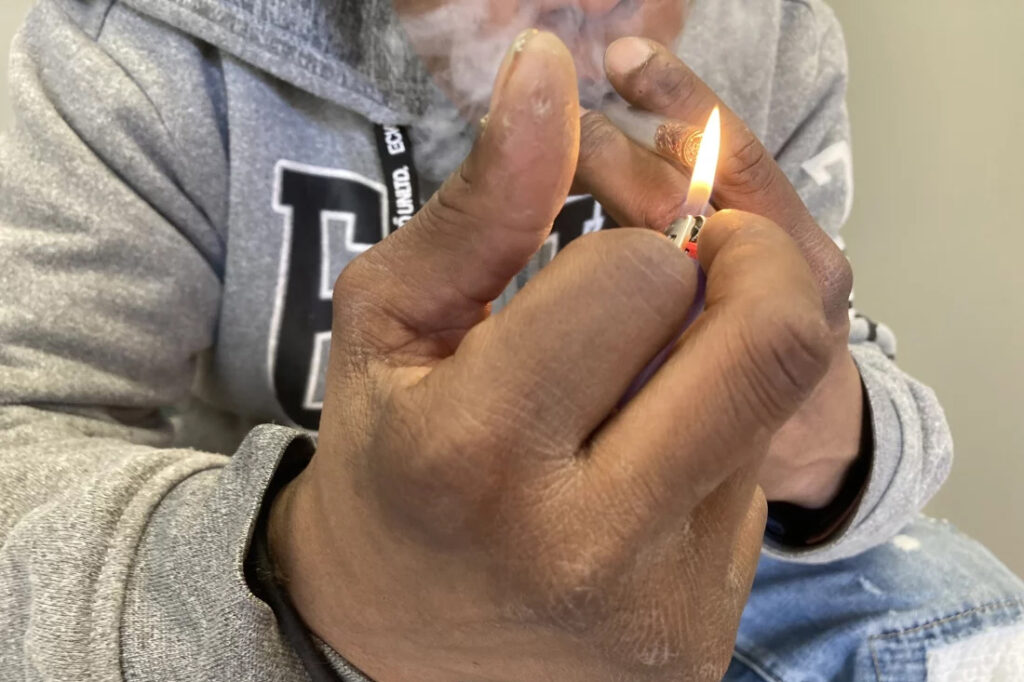
In Pawtucket, Rhode Island, near a storefront advertising “free” cellphones, J.R. sat in an empty back stairwell and showed a reporter how he tries to avoid overdosing when he smokes crack cocaine. KFF Health News is identifying him by his initials because he fears being arrested for using illegal drugs.
It had been several hours since his last hit, and the chatty, middle-aged man’s hands moved quickly. In one hand, he held a glass pipe. In the other, a lentil-size crumb of cocaine.
Or at least J.R. hoped it was cocaine, pure cocaine — uncontaminated by fentanyl, a potent opioid that was linked to about 75% of all overdose deaths in Rhode Island in 2022. He flicked his lighter to “test” his supply. He believed that if it had a “cigar-like sweet smell,” he said, it would mean that the cocaine was laced with fentanyl. He put the pipe to his lips and took a tentative puff. “No sweet,” he said, reassured.
But this method offers only false and dangerous reassurance. A mistake can be fatal.
It is impossible to tell whether a drug contains fentanyl by the taste or smell. “Somebody can believe that they can smell it or taste it, or see it … but that’s not a scientific test,” said Josiah “Jody” Rich, an addiction specialist and researcher who teaches at Brown University. “People are going to die today because they buy some cocaine that they don’t know has fentanyl in it.”
The first wave of the long-running and devastating opioid epidemic began in the United States with the abuse of prescription painkillers in the early 2000s. The second wave involved an increase in heroin use, starting around 2010. The third wave began when powerful synthetic opioids such as fentanyl started appearing in the supply around 2015. Now experts are observing a fourth phase of the deadly epidemic.
The mix of stimulants such as cocaine and methamphetamines with fentanyl — a synthetic opioid 50 times as powerful as heroin — is driving what experts call the opioid epidemic’s “fourth wave.” The mixture of stimulants and fentanyl presents powerful challenges to efforts to reduce overdoses because many users of stimulants don’t know they are at risk of ingesting opioids, so they don’t take overdose precautions.
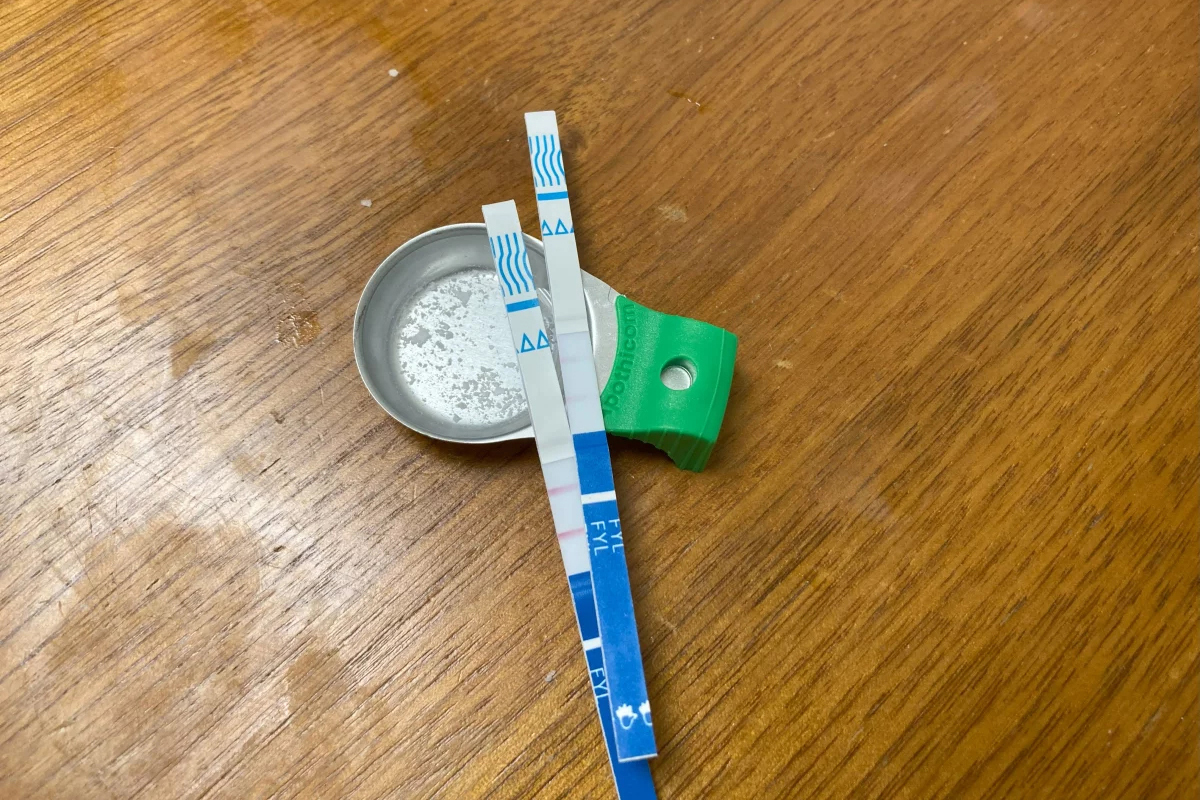
The only way to know whether cocaine or other stimulants contain fentanyl is to use drug-checking tools such as fentanyl test strips — a best practice for what’s known as “harm reduction,” now embraced by federal health officials in combating drug overdose deaths. Fentanyl test strips cost as little as $2 for a two-pack online, but many front-line organizations also give them out free.
Nationwide, illicit stimulants mixed with fentanyl were the most common drugs found in fentanyl-related overdoses, according to a study published in 2023 in the scientific journal Addiction. The stimulant in the fatal mixture tends to be cocaine in the Northeast, and methamphetamine in the West and much of the Midwest and South.
“The No. 1 thing that people in the U.S. are dying from in terms of drug overdoses is the combination of fentanyl and a stimulant,’’ said Joseph Friedman, a researcher at UCLA and the study’s lead author. “Black and African Americans are disproportionately affected by this crisis to a large magnitude, especially in the Northeast.”
Friedman was also the lead author of another new study, published in the American Journal of Psychiatry, that shows the fourth wave of the opioid epidemic is driving up the mortality rate among older Black Americans (ages 55-64) and, more recently, Hispanic people. Friedman said part of the reason street fentanyl is so deadly is that there’s no way to tell how potent it is. Hospitals have safely used medical-grade fentanyl for surgical pain because the potency is strictly regulated, but “the potency fluctuates wildly in the illicit market” Friedman said.
Studies of street drugs, he said, show that in illicit drugs the potency can vary from 1% to 70% fentanyl.
“Imagine ordering a mixed drink in a bar and it contains one to 70 shots,” Friedman said, “and the only way you know is to start drinking it. … There would be a huge number of alcohol overdose deaths.”
Drug-checking technology can provide a rough estimate of fentanyl concentration, he said, but to get a precise measure requires sending drugs to a laboratory.
It’s not clear how much of the latest trend in polydrug use — in which users mix substances, such as cocaine and fentanyl, for example — is accidental versus intentional. It can vary for individual users: a recent study from Millennium Health found that most people who use fentanyl do so at times intentionally and other times unintentionally.
People often use stimulants to power through the rapid withdrawal from fentanyl, Friedman said. And the high-risk practice of using cocaine or meth with heroin, known as “speedballing,” has been around for decades. Other factors include manufacturers’ adding the cheap synthetic opioid to a stimulant to stretch their supply, or dealers mixing up bags.
Researchers say many people still think they are using unadulterated cocaine or crack — a misconception that can be deadly. “Folks who are using stimulants, and not intentionally using opioids, are unprepared to respond to an opioid overdose,” said Brown University epidemiologist Jaclyn White Hughto, “because they don’t perceive themselves to be at risk.” Hughto is a principal investigator in a new, unpublished study called “Preventing Overdoses Involving Stimulants.”
Hughto and the team surveyed more than 260 people in Rhode Island and Massachusetts who use drugs, including some who manufacture and distribute stimulants such as cocaine. More than 60% of the people they interviewed in Rhode Island had bought or used stimulants that they later found out had fentanyl in them. And many of the people interviewed in the study also use drugs alone. That means that if they do overdose, they may not be found until it’s too late.
In 2022, Rhode Island had the fourth-highest rate of overdose deaths involving cocaine in 2022, after Washington, D.C., Delaware, and Vermont, according to the Centers for Disease Control and Prevention.
The fourth wave is also hitting stimulant users who choose pills over what they perceive as more dangerous drugs such as cocaine in an effort to avoid fentanyl. That’s what happened to Jennifer Dubois’ son Cliffton.
Dubois was a single mother raising two Black sons. The older son, Cliffton, had been struggling with addiction since he was 14, she said. Cliffton also had been diagnosed with attention-deficit/hyperactivity disorder and a mood disorder.
In March 2020, Cliffton had checked into a rehab program as the pandemic ramped up, Dubois said. Because of the lockdown at rehab, Cliffton was upset about not being able to visit with his mother. “He said, ‘If I can’t see my mom, I can’t do treatment,’” Dubois recalled. “And I begged him” to stay in treatment.
But soon after, Cliffton left the rehab program. He showed up at her door. “And I just cried,” she said.

Dubois’ younger son was living at home. She didn’t want Cliffton doing drugs around his younger brother. So she gave Cliffton an ultimatum: “If you want to stay home, you have to stay drug-free.”
Cliffton went to stay with family friends, first in Atlanta and later in Woonsocket, an old mill city that has Rhode Island’s highest rate of drug overdose deaths.
In August 2020, Cliffton overdosed but was revived. Cliffton later confided that he’d been snorting cocaine in a car with a friend, Dubois said. Hospital records show he tested positive for fentanyl.
“He was really scared,” Dubois said. After the overdose, he tried to “leave the cocaine and the hard drugs alone,” she said. “But he was taking pills.” Eight months later, on April 17, 2021, Cliffton was found unresponsive in the bedroom of a family member’s home.
The night before, Cliffton had bought counterfeit Adderall, according to the police report. What he didn’t know was that the Adderall pill was laced with fentanyl. “He thought by staying away from the street drugs and just taking pills, he was doing better,” Dubois said.
A fentanyl test strip could have saved his life.

This article is from a partnership that includes The Public’s Radio, NPR, and KFF Health News.
[ad_2]
Source link